Well, you will find this hard to believe, but your thyroid medication could actually be causing you more harm than good. Have you noticed these symptoms with your thyroid disorder?
- Tiredness.
- More sensitivity to cold.
- Constipation.
- Dry skin.
- Weight gain.
- Puffy face.
- Hoarse voice.
- Coarse hair and skin.
- Muscle weakness.
- Muscle aches, tenderness and stiffness.
- Menstrual cycles that are heavier than usual or irregular.
- Thinning hair.
- Slowed or racing heart rate.
- Depression.
- Memory problems.
- Anxiety
Now let's check out the symptoms of taking levothyroxine.
Levothyroxine is a prescription drug. It comes as a tablet or capsule you take by mouth. It also comes as an injectable solution that’s only given by a healthcare provider.
Levothyroxine oral tablet is available as the brand-name drugs Levoxyl, Synthroid, and Unithroid.
Levothyroxine oral tablet can cause side effects.
More common side effects
The more common side effects of levothyroxine can include:
Serious side effects
Call your doctor right away if you have serious side effects. Call 000 if your symptoms feel life threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
- Heart attack. Symptoms can include:
- chest pain
- shortness of breath
- discomfort in your upper body
- Heart failure. Symptoms can include:
- shortness of breath
- extreme tiredness
- swelling in your legs, ankles, or feet
- unexpected weight gain
- Very fast heart rate
- Irregular heart rhythm
This what you get when taking synthetic drugs.
My suggestion would be to try natural bovine supplements.
As we deal with global uncertain times, our way of life has shifted dramatically and stress levels are at an all-time high. The disruption of our routines and the uncertainty of what’s to come is undoubtedly stressful, and for some, spiked stress levels can disrupt the hair’s natural growth cycle, which may lead to excessive shedding and hair loss.
Hair loss can be caused by an imbalance in hormone levels. Cortisol is one of the hormones often identified with hair loss. Understanding how hormones and hair loss are connected and how to regulate the effects can help lead to healthier hair.
WHAT IS CORTISOL?
Cortisol is a steroid hormone, one of the glucocorticoids made in the cortex of the adrenal glands which is released into the blood and transported throughout the body. Most cells contains receptors for cortisol which can have many different actions depending on which sort of cells it acts upon. These effects include controlling the body’s blood sugar levels and thus regulating metabolism, acting as an anti-inflammatory, influencing memory formation, controlling salt and water balance, regulating blood pressure, and helping foetal development during pregnancy. All of these functions make cortisol a crucial hormone to protect overall health and wellbeing.
HOW HORMONES AND HAIR LOSS ARE CONNECTED THROUGH STRESS
Extended stress leads to longer periods of high cortisol levels. While the adrenal glands are busy making extra cortisol, they make less of the hormones which support healthy hair growth. Sustained high cortisol levels can also lead to other health problems, including a decrease in cell regeneration, impaired mental function, decreased metabolism, and a weakened immune system.
Cortisol is known to affect the function and cyclic regulation of the hair follicle. During periods of stress, cortisol dysregulation can disrupt cell signaling, and oxidative stress can disrupt the normal transitions of the hair growth cycle. In-vitro studies have demonstrated that proinflammatory cytokines, including tumor necrosis factor-alpha (TNF?), interleukin (IL)-1?, and IL-1?, cause the formation of vacuoles within hair matrix cells as well as abnormal keratinization of the inner root sheath and follicle bulb and inner root sheath. These cytokines have also been shown to disrupt follicular melanocytes and promote the formation of melanin granules within the dermal papilla. They can disturb the hair cycle, which may cause premature arrest of hair cycling. Specifically, these molecules can prevent the hair growth cycle from moving from the telogen phase to the anagen growth phase.
There are three types of hair loss which can all be associated with high stress levels:
- Telogen effluvium (TEL-o-jun uh-FLOO-vee-um), where a significant stress pushes large numbers of hair follicles into a resting phase. Within a few months, affected hairs might fall out suddenly when simply combing or washing hair
- Trichotillomania (trik-o-til-o-MAY-nee-uh), an irresistible urge to pull hair out from the scalp, eyebrows, or other areas of the body. Hair pulling can be a way of dealing with negative or uncomfortable feelings, such as stress, tension, loneliness, boredom, or frustration
- Alopecia areata (al-o-PEE-she-uh ar-e-A-tuh) is when the body’s immune system attacks the hair follicles, causing hair loss. This is thought to be caused by a variety of factors, possibly including severe stress
TESTING FOR STRESS-RELATED HAIR LOSS
Dried Urine Cortisol testing is a non-invasive collection method. It is used as a diagnostic tool to identify chronic stress disorders and may also be useful in understanding stress-related hair loss. This testing is part of the DUTCH Complete™ panel offerings.
The DUTCH Plus® uses four dried urine samples and five saliva samples. These samples are collected over the course of one day, from waking to bed time, and includes three Cortisol Metabolites and the diurnal pattern of Free Cortisol and Cortisone, including the Cortisol Awakening Response (CAR) with a saliva measurement.
What is a Lipotropic?
Lipotropic compounds are key within the metabolism, transport and breakdown of fat in the body.
In particular, they play an important role in the removal of excess fats and fat-soluble compounds (including hormones and toxins) from the liver.
Beyond the fundamental support for bile production and lipid metabolism provided by Taurine, Glycine and Inositol, Acetyl-Carnitine can provide additional support by facilitating the ferrying of lipid compounds into mitochondria for beta-oxidation.
Beta-oxidation provides an important source of metabolic energy, particularly during periods of weight loss and between meals, as well as high energy demand states, such as exercise and stress. These metabolic conditions induce the release of fatty acids from adipose tissue, due to the secretion of circulating mediators such as glucagon and the adrenal hormone epinephrine, which increase the rate of lipolysis.
Fatty acid oxidation thus constitutes a high-efficiency alternate method of energy production, i.e. through the conversion of acetyl-COA to ATP in muscles, and the production of ketones from fats in the liver. This can help spare muscles from catabolic breakdown, as well as minimise excess fat accumulation and congestion.
Choline is another important nutrient involved in fat metabolism. Choline functions as a methyl donor and is required for numerous aspects of liver function. Even though choline can be synthesised from methionine, evidence suggests that choline is an essential nutrient itself.
Methionine is therefore sometimes included with lipotropic nutrient supplements, however methionine can put an increased demand on methylation nutrient reserves in order to recycle it from homocysteine. (Otherwise, the homocysteine would accumulate). It is therefore potentially more prudent to avoid exogenous methionine supplementation, leaving adequate supplies to be maintained through folate and vitamin B12 (methylation) status alone.
Lipotropics are necessary nutrients for the maintenance of a healthy liver, and also the body as a whole. Without lipotropics, fats and bile can become trapped in the liver, which may be involved in hepatic issues such as cirrhosis, NAFLD, NASH as well as compromised fat metabolism overall.
Lipotropics differ from Cholagogues and Choleretics (which simply trigger the release and production of bile respectively), by providing the actual substrates necessary to produce the bile. Lipotropics also conjugate the lipid compounds needing excretion (via bile) and metabolise associated lipid compounds to energy and by-products.
These properties give lipotropics a very broad range of clinical uses and applications, and make their inclusion within a wide range of clinical programs almost universally beneficial and well tolerated.
Why are Lipotropics so powerful for treating liver health?
Phase 2 liver pathways are responsible for processing the following compounds;
Prostaglandins
Leukotrienes
Alcohol
Paracetamol
Heavy Metals
Petro-chemicals
Mould Toxins
Bacterial Toxins
Steroid Hormones
(DHEA, Oestro, T,
25-OH-Vitamin D)
Thyroxine
Amines (Tryp, Tyr)
Cortisol
Epinephrine
Melatonin
Steroid Hormones
(Oestro, T, Prog…)
Fat Soluble Vits
(Vit A, D, E, K)
Fat Soluble Toxins
(Pesticides – DDT)
Thyroxine
Melatonin
Neurotransmitters
Serotonin
Histamine
Choline
Amines (Tryp, Tyr)
Phenols
Caffeine
CoA
Bile Acids
Salicylates
Benzenes
SCFAs
MCFAs
Bacterial Toxins
—-
—-
Neurotransmitters
L-Dopa/Dopamine
Nor/Epinephrine
Histamine
OH-Oestrogens
Heavy Metals
(Hg, Pb, Cd, As)
Morphine
If optimum liver function is compromised and obstructed, many of these compounds may not be metabolised effectively and efficiently, potentially resulting in widespread impairments to the body’s normal biochemical pathways.
Lipotropics are responsible for bile production, and bile is key to facilitating the ejection of Phase 2 Liver conjugates into the gut lumen for proper excretion from the body. Therefore, Lipotropics are essential for supporting all Phase 2 detoxification processes.
In particular, fat-soluble compounds requiring detoxification (such as hormone excesses as well as modern chemical toxins and mould toxins) will need adequate bile flow and lipid metabolism capabilities to be dealt with.
In modern society, congested liver function is a common occurrence, with diets high in alcohol, excess sugar and fructose, as well as stress and lack of exercise contributing to chronic liver dysfunction and fat accumulation.
If you are a male, you have likely heard or read about declining testosterone (low T). Testosterone production does decrease with age, but it can also decrease faster from poor lifestyle choices, chemicals in the environment, and conditions such as obesity and diabetes. This creates a host of symptoms such as low sex drive, poor sexual function, decreased muscle mass or the inability to increase it, anxiety, slow healing, low motivation, and more.
While declining testosterone in men is definitely a problem, we also know oestrogen can be just as important when it comes to hormone balance as a man ages. Researchers have discovered that just as women go through menopause due to a dramatic decrease in oestrogen product, middle-aged men also undergo oestrogen-related changes in body composition and sexual function.
A study published in The New England Journal of Medicine was conducted by researchers at Massachusetts General Hospital (MGH) which found that a diagnosis of male hypogonadism (a drop in reproductive hormone levels high enough to cause physical symptoms) is traditionally made based on blood testosterone levels. However, there is little understanding of the levels of testosterone needed to support certain functions.
ACCORDING TO THE STUDY AUTHORS, A SMALL PROPORTION OF THE TESTOSTERONE MADE BY MEN IS USUALLY CONVERTED INTO OESTROGEN BY AROMATASE, A TYPE OF ENZYME, AND THE HIGHER THE TESTOSTERONE LEVEL IN A MAN, THE MORE TESTOSTERONE IS CONVERTED INTO OESTROGEN.
If the aromatase enzyme is upregulated, a man will become oestrogen dominant. The major clinical signs of oestrogen excess in men are gynaecomastia (breast development), testicular atrophy, erectile dysfunction, depression, and infertility (1). Another potential effect includes a significantly increased risk for type-2 diabetes (2, 3). We know excess oestrogen also causes water retention (less frequent urination) in both men and women, which can lead to excessive sweating, blood pressure spikes or high blood pressure, insomnia, hot flushing around the ears or on the face, night sweats, and brain fog.
On the flip side, what if men do not have enough oestrogen? Oestrogen is required for the activation of testosterone receptors and, in the presence of very low oestrogen this triggers, a loss of testosterone receptors. This decline in the number of testosterone receptors can have a dramatic impact the body because testosterone will not have anywhere to bind and create action. In the same study referenced above, authors developed a testing method using various combinations of testosterone, oestrogen, anastrozole, and goserelin acetate and found that “oestrogen deficiency primarily accounted for increases in body fat, and both contributed to the decline in sexual function” (4). This data confirms that testosterone is not the only important player when it comes to men’s sexual and overall health. Another study shows cortical bone is depleted when oestrogen levels are low (5). This puts men at risk for osteoporosis.
Once again, it is the balance of testosterone and oestrogen that is important! For a long time medical professionals have thought oestrogen is detrimental to a man’s well-being, but we now know that is not entirely true.
Men should test their hormone levels to detect and correct imbalances associated with symptoms. Testosterone and its metabolites and oestrogen metabolism are all reported on the male sex hormone pages of the DUTCH Test®. This allows practitioners to fully evaluate the androgens such as DHEA-S, testosterone, 5a-DHT, 5a and 5b-androstanediol, etiocholanolone, and androsterone. In addition, the three main oestrogens (oestrone, oestradiol, and oestriol) plus oestrogen metabolism will show if a male patient is oestrogen dominant or oestrogen deficient and how his oestrogen detoxification is working. Better patient outcomes can be achieved when evaluating these two hormone sections in tandem.
Image: The pathways of Oestrogens and Androgens and associated metabolites in the DUTCH test.
References
[1] Estrogen and the Male, Judy K. Lee, Julianne Imperato-McGinley, in Encyclopedia of Endocrine Diseases, 2004.
[2] Diabetes Care. 2013 Sep; 36(9): 2591–2596. Published online 2013 Aug 13. doi: 2337/dc12-2477.
[3] Circulating Estrone Levels Are Associated Prospectively With Diabetes Risk in Men of the Framingham Heart Study, Guneet Kaur Jasuja, PHD,1,2 Thomas G. Travison, PHD,3,4 Maithili Davda, MPH,3 Adam J. Rose, MD,2,5 Anqi Zhang, PHD,3 Mark M. Kushnir, PHD,6 Alan L. Rockwood, PHD,6 Wayne Meikle, MD,6 Andrea D. Coviello, MD, MS,3,7 Ralph D’Agostino, PHD,1,2 Ramachandran S. Vasan, MD,7,8 and Shalender Bhasin, MD3
[4] Gonadal Steroids and Body Composition, Strength, and Sexual Function in Men, Joel S. Finkelstein, M.D., Hang Lee, Ph.D., Sherri-Ann M. Burnett-Bowie, M.D., M.P.H., J. Carl Pallais, M.D., M.P.H., Elaine W. Yu, M.D., Lawrence F. Borges, M.D., Brent F. Jones, M.D., Christopher V. Barry, M.P.H., Kendra E. Wulczyn, B.A., Bijoy J. Thomas, M.D., and Benjamin Z. Leder, M.D., N Engl J Med 2013; 369:1011-1022 September 12, 2013DOI: 10.1056/NEJMoa1206168.
[5] Serum estradiol levels are inversely associated with cortical porosity in older men. Vandenput L1, Lorentzon M, Sundh D, Nilsson ME, Karlsson MK, Mellström D, Ohlsson C.,J Clin Endocrinol Metab. 2014 Jul;99(7):E1322-6. doi: 10.1210/jc.2014-1319. Epub 2014 Apr 2.
[6] The effect of estrogen and androgen on androgen receptors and mRNA levels in uterine leiomyoma, myometrium and endometrium of human subjects. Fujimoto J1, Nishigaki M, Hori M, Ichigo S, Itoh T, Tamaya T., J Steroid Biochem Mol Biol. 1994 Aug;50(3-4):137-43.
[7] The role of estradiol in male reproductive function, Michael Schulster,1 Aaron M Bernie,1 and Ranjith Ramasamy 2 J Clin Endocrinol Metab. 2014 Jul;99(7):E1322-6 doi: 10.1210/jc.2014-1319. Epub 2014 Apr 2.
Chronic stress is all too prevalent and it can be a significant impediment to disease prevention and optimal health.
Stress increases cortisol which may have a profound impact on the gastrointestinal (GI) microbiota and metabolome, selectively decreasing beneficial bacteria and secretory IgA (sIgA). Thus, it is not surprising that clinical interventions implemented to resolve GI symptoms may not be completely successful if stress is not considered as a potential root cause.
Chronic stress directly effects our gastrointestinal health via hypothalamic-pituitary-adrenal (HPA) axis activation. Stress can adversely affect GI bacteria and secretory IgA (sIgA), which may influence intestinal permeability, and selectively decrease beneficial bacterial species.
CHRONIC STRESS WILL DOWN REGULATE FAECAL sIgA, WHICH INCREASES THE RISK OF GI INFECTION
Animal models have provided insight into stress and its effects on the GI microbiome. Stress caused by maternal separation of rhesus monkeys changed their microbiome via decreased Bifidobacterium and Lactobacillus. Rat pups separated from their mother exhibited decreased Lactobacillus levels which was maintained for an extended period of time. As such, acute and chronic stress may lead to the development of intestinal dysbiosis and chronic low grade inflammation. Gastrointestinal dysbiosis and chronic low-grade inflammation have been implicated in IBS and depression.
Chronic stress weakens the intestinal mucosal barrier and permits paracellular bacterial translocation from the lumen. This stimulates the activation of the inflammatory meditators, resulting in activation of the HPA axis.
OUR MODERN LIFESTYLES OFTEN LEAD TO THE DEVELOPMENT OF CHRONIC STRESS AND FURTHER SYSTEMIC SYMPTONS IN THE FORM OF INCREASED HPA AXIS ACTIVATION, INCREASED FAECAL SIGA, DISTURBANCES IN THE GI MICROBIAL COMPOSITION AND INCREASED INTESTINAL PERMEABILITY.
Clinicians can evaluate levels of faecal sIgA, the GI microbiota, and intestinal permeability to gain insight into potentially confounding roles of stress on GI and systemic symptoms. Testing HPA axis function and neurotransmitter secretion can be an important tool in helping to address the imbalances that can result from long term chronic stress. Stress management should be considered as part of a comprehensive clinical intervention.
The interplay between stress, the HPA axis and the gastrointestinal system is complex and intricate, while the impacts on human physiology are vast.
– By Julia Malkowski, ND, DC
Sign up and log in for an account https://benjaminmcavoy.com/shop/
How using the right form of Magnesium could be the missing piece of your treatment puzzle.
As A functional medicine practitioner, I often look to how I can support not just one area of the body, but how different areas of the body interact with each other and what tools we can use to maximise healing and wellness overall.
Magnesium supports over 300 biological reactions in the body, including energy production, the regulation of blood pressure and anti-inflammatory processes, it is no surprise that it is one of the most common nutrients prescribed generally.
Magnesium in Osteopathic Treatment
Magnesium has been shown to have positive effects on the bone mineral density of both men and women, and is involved in bone formation, influencing the activity of osteoblasts and osteoclasts.
When it comes to many pain-related issues resulting from severe inflammation of the body, magnesium can assist with pain management due to its anti-inflammatory benefits. It can therefore play a role in the treatment of issues such as back pain, neck pain, whiplash, overuse injuries and sports related recovery.
When it comes to the recovery of sport related issues, magnesium can assist with relieving lactic acid build up in muscles and promoting the production of protein within the body, resulting in a more effective recovery process.
Signs of Magnesium Deficiency
Those who are deficient may suffer from chronic muscle pain and spasms, low energy, headaches and digestive issues. Although research has shown that we can see amazing benefits from magnesium supplementation even if we are not clinically deficient.
What Form of Magnesium is Best?
Magnesium can be found in many different and varying chemical forms. Some forms are better absorbed by the body, and are therefore more effective than others. On the other hand, some forms of magnesium can target specific areas of the body better than others. Below is a quick comparison of when you might prescribe one form over another, or even combine multiple forms, to maximise various uptake mechanisms.
Magnesium Citrate
A form of citric acid and one of the most commonly used forms of magnesium, the highly absorbed magnesium citrate is known for its calming effects and is used to help soothe muscle cramps and the nervous system, in turn helping to relieve symptoms of stress, anxiety & restlessness.
As citric acid is a mild form of laxative, magnesium citrate is sometimes used to assist with digestive issues such as constipation. Additionally, if you have patients often struggling with fatigue, magnesium citrate assists with helping the body to metabolise energy.
Recommend purpose: Magnesium Citrate is a more well-rounded form of magnesium for general wellbeing. It is helpful for calming the nervous system and muscle cramps.
Magnesium L-Threonate
Magnesium L-Threonate is an easily absorbed, extremely bioavailable form of magnesium, and is the optimum form for supporting brain and nervous system health.
Magnesium L-Threonate is known for its ability to readily cross the blood brain barrier thus serving as a neurological cofactor in cognitive, mood and stress related functions.
Therefore, it is the best form for increasing magnesium levels in the brain cells, in turn assisting with the management of brain disorders such as age-related memory loss, depression and stress related symptoms.
Recommend purpose: Magnesium L-Threonate is effective for the management of brain related support and nervous function.
Magnesium Glycinate
Formed from elemental magnesium and the amino acid glycine, magnesium glycinate is a calming agent and is most commonly used as a dietary supplement to help improve sleep and treat symptoms of anxiety.
Magnesium Glycinate is also used to help support a range of inflammatory diseases and chronic disorders such as diabetes. Magnesium Glycinate is the form most unlikely to cause irritations of the bowel such as diarrhoea, therefore is the most effective source of magnesium for long-term consumption.
Recommend purpose: Magnesium Glycinate is effective for the management of inflammatory disease, as well as maintaining nervous system function. Magnesium glycinate is recommended to help manage symptoms of depression, anxiety and stress.
Magnesium Orotate
Magnesium Orotate is an easily absorbed form of magnesium that includes orotic acid.
Orotic acid is a natural substance involved in the process of the body’s construction of genetic material such as DNA. A popular form amongst athletes, magnesium orotate assists in the process of moving blood sugar into fatigued muscles, in turn assisting in the elimination lactate. This assists those with physical jobs, athletes or fitness enthusiasts and supports the recovery of their bodies, resulting in a more efficient recovery time.
Recommend purpose: Magnesium Orotate is the recommended form of magnesium to help support the recovery of athletes, those with physical jobs and fitness enthusiasts.
Summary
Using different forms of magnesium can be a great tool in your treatment tool box – just make sure you’re using a form (or forms) that is not only highly bioavailable but also the optimal form for your specific patient needs.
Please contact me if you wish to purchase the best Magnesium for your body,
Sign up and log in for an account https://benjaminmcavoy.com/shop/
Mycotoxins are toxic chemicals that are naturally produced by fungi like mould, which can infest buildings, vehicles, and foodstuffs.
The majority of mycotoxin exposures are through food ingestion or airborne exposure. In fact, mycotoxins are estimated to contaminate 25 percent of the world’s crops.
Damp climates, insect damage, and poor food storage facilitate the growth of mould and hence increase the likelihood and levels of mycotoxin contamination.
A recent study done by the Environmental European Commission earlier this year found that 5 percent of hazelnuts showed ochratoxin (a nephrotoxic, immunotoxic, and carcinogenic mycotoxin) contamination, while 10 percent of dried grapes, 20 percent of dried figs, and 50 percent of pistachios imported from Turkey showed aflatoxin contamination.
Aflatoxin exposure has been correlated with cancer, mental impairment, and liver damage – and is said to be responsible for 28 percent of all liver cancers in the world.
The Link Between Mycotoxins & Disease
Mycotoxins are absorbed in the mucosal epithelia in the airways and the gut and can affect many immune-related organs and cell types.
These interactions suppress immune functions. Multiple types of mycotoxins can cause a decrease in B cells, white blood cells, and hematopoietic stem cells. Exposure to mycotoxins decreases the amount of mature CD4+ cells and splenic T lymphocytes.
This exposure will also affect different groups of cytokines. IL-2 production and IL-2 receptors are decreased, but IL-17, IL10, TGF-a, and MIP-1b are all elevated. These changes in cytokine expression can lead to enhanced tissue damage to multiple different tissues and organs.
Common Mould Markers and their Effects
Aflatoxin
- Sources – Beans, Corn, Rice, Tree Nuts, Wheat, Milk, Eggs, Meal
- Impacts – Liver Damage, Mental Impairment, Abdominal Pain, Jaundice, Headache
Ochratoxin
- Sources – Food & Water-Damaged Buildings
- Impacts – Kidney Function, Neurological Symptoms, Immune Suppression
Sterigmatocystin
- Sources – Grains, Corn, Bread, Cheese, Coffee Beans, Dust from Damp Carpets
- Impacts – Liver Damage, Kidney Damage, Immune Suppression
Roridin E
- Sources – Water-Damaged Buildings, Contaminated Grain
- Impacts – Neurological Damage, GI Distress, Cardiovascular Problems, Endocrine Disruption, Immune Suppression
Verrucarin A
- Sources – Water-Damaged Buildings, Contaminated Grain
- Impacts – Vomiting, Weight Loss, Skin Dermatitis, Nervous Disorders, Reproductive Problems, Immunosuppression
Enniatin B
- Sources – Contaminated Grain
- Impacts – Weight Loss, Fatigue, Liver Damage
Zearalenone
- Sources – Wheat, Barley, Rice, Corn
- Impacts – Reproductive Effects (Disrupts Conception, Ovulation Foetal Development)
Gliotoxin
- Sources – Cereal Crops, Spices, Eggs, Milk, Meat
- Impacts – Neurological Symptoms, Immunosuppression, Liver Function
Mycophenolic Acid
- Sources – Citrus Fruits, Seeds, Grains
- Impacts – Immunosuppression, Birth Defects
Citronin
- Sources – Wheat, Rice, Corn, Flour
- Impacts – Kidney Damage, Immunosuppression
Chaetoglobosin A
- Sources – Water-Damaged Buildings
- Impacts – Gastrointestinal Disorders, Disrupted Cellular Division
How to Reduce and Remove Mycotoxins
Reducing exposure to mould remains the greatest priority when trying to minimise the effects of mycotoxins on the body. The main sources of exposure include:
Food
If foods are the main source of exposure then removing culprit foods is the primary method to reduce overall mycotoxin exposure. Testing for the exact mycotoxins can verify if food is the primary source of mould exposure and which foods, in particular, may be of concern.
Lifestyle & Environment
An individual’s environment can be one of the greatest contributors to their mycotoxin load. Finding and removing any sources of mould in the house, transport and any other places can often be the first step to reducing the impact of mould.
Testing and Treatment for Mould
Testing
Testing remains the most accurate way to determine the presence of mould, alongside exactly what mould markers are present. Knowing the mould markers can narrow down the source of exposure and help choose the most accurate treatment strategies for that individual.
Strategies to reduce Mould
- Hydration – Mycotoxins need adequate levels of water to be fully eliminated from the body, regardless of whether they’re being removed by endogenous detoxification processes, exercise and sweating or supplements.
- Binders – Due to their inert and non-reactive nature, binders can be the supplement of choice for individuals with mould exposure who may also be experiencing allergies and sensitivities to products. Binders can preferentially adsorb and eliminate mycotoxins without interacting with nutrients, the microbiome and other cells in the body.
- Anti-Inflammatory and Antioxidant nutrients – As the main impacts of mycotoxins include suppression of immunity, alongside an increase in inflammation and oxidative stress, anti-inflammatory and antioxidant herbs and nutrients can be specifically beneficial for mycotoxin exposure.
- Exercise and Sweating – Sweating and movement can be one of the most effective ways to eliminate mycotoxins.
Highlights
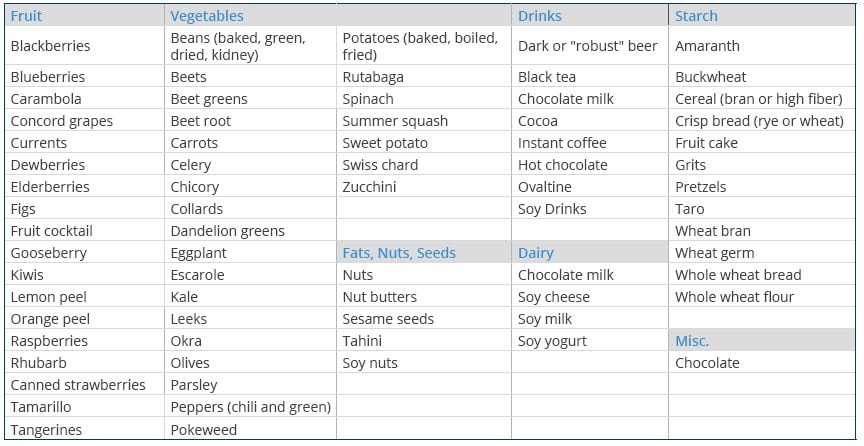
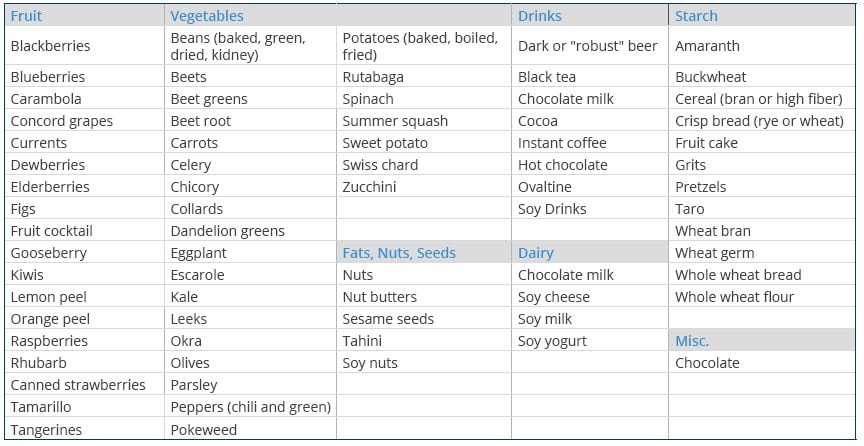
- Oxalates are a potentially harmful compound found in many foods (such as leafy greens) otherwise known as healthy.
- Too-high levels may lead to a range of conditions including kidney stones and systemic inflammation.
Introduction
Green smoothie for breakfast, tofu salad with nuts for lunch, and baked potatoes and grains for dinner. As healthy as this meal plan sounds, there is one potentially harmful compound that such a meal plan is extremely high in – and that is oxalates.
What are Oxalates?
Oxalates and their acidic form oxalic acid is one of the most acidic compounds in the human body. Found as part of cellular reactions, a by-products of yeasts and fungus and other microorganisms, oxalates also enter the body through food.
When do Oxalates Become an Issue?
Oxalates may become an issue for those with a diet high in plant-based foods. Oxalates can form crystals throughout the body including in bones, joints, blood vessels, lungs, thyroid, and even the brain. These crystals are sharp in nature, and very high levels may result in increased pain and inflammation throughout the body.
High levels of oxalates are considered to be especially dangerous for those with a history of kidney stones as they can result in the formation of a certain type of stone. However, ongoing research has linked high levels of oxalates to a range of other health conditions.
Where are they found?
Oxalates are found among a wide range of foods including:
How to reduce oxalates?
- Diet Modification – Low oxalate diet
- Hydration – Drinking enough liquids helps eliminate oxalates from the body.
- Fat Digestion – Excessive fats in diet may lead to increased oxalates. Supporting fat digestion can help reduce overall oxalate load.
- Omega 3s – Increase intake of essential omega-3 fatty acids, commonly found in fish oil and cod liver oil, which reduces oxalate problems. High amounts of the omega-6 fatty acid, arachidonic acid, are associated with increased oxalate problems. Meat from grain fed animals is high in arachidonic acid.
Testing for Oxalates
The Great Plains Laboratory Organic Acids Test (OAT) test for multiple markers connected with oxalates including Glyceric Acid, Glycolic Acid and Oxalic Acid. Message me here to order an OAT test
Treating High Oxalate Levels
- Antifungal Medications – Use antifungal drugs to reduce yeast and fungi that may be causing high oxalates. Children with autism frequently require years of antifungal treatment. Arabinose, a marker used for years for yeast/fungal overgrowth in the Organic Acids Test is correlated with high amounts of oxalates.
- Calcium and Magnesium – Supplements of calcium and magnesium citrate can reduce oxalate absorption from the intestine. Citrate is the preferred calcium form to reduce oxalate because citrate also inhibits oxalate absorption from the intestinal tract.
- Glucosamine – N-Acetyl glucosamine supplements can stimulate the production of the intercellular cement, hyaluronic acid, to reduce pain caused by oxalates.
- Chondroitin – Chondroitin sulfate can prevent the formation of calcium oxalate crystals.
- B6 – Vitamin B6 is a cofactor for one of the enzymes that degrades oxalate in the body and has been shown to reduce oxalate production.
- Taurine – Excessive fats in the diet may cause elevated oxalates if the fatty acids are poorly absorbed because of bile salt deficiency. If taurine is low, supplementation with taurine may help stimulate bile salt production (taurocholic acid), leading to better fatty acid absorption and diminished oxalate absorption.
- Probiotics – Probiotics may be very helpful in degrading oxalates in the intestine. Individuals with low amounts of oxalate-degrading bacteria are much more susceptible to kidney stones. Both Lactobacillus acidophilus and Bifidobacterium lactis have enzymes that degrade oxalates.
- Other Nutrients – Supplements of vitamin E, selenium, and arginine have been shown to reduce oxalate damage.
 Abstract
Abstract
Background: We aimed to investigate the link of vitamin C status with vitality and psychological functions in a cross-sectional study, and examine their causal relationship through a randomised controlled trial (RCT).
Methods: We first conducted a population-based cross-sectional investigation of healthy young adults (n = 214, 20–39 years), and analyzed the associations of serum vitamin C concentrations with vitality (fatigue and attention) and mood status (stress, depression, and positive and negative affect) using Pearson’s correlation and multiple linear regression analyses. Next, we performed a double-blind RCT in healthy subjects whose serum vitamin C concentrations were inadequate (< 50 umol/L). Subjects were randomly allocated to receive 500 mg of vitamin C twice a day for 4 weeks (n = 24) or a placebo (n = 22). We assessed vitality, which included fatigue, attention, work engagement, and self-control resources, and measured mood status, including stress, depression, positive and negative affect, and anxiety. ELISA determined serum brain-derived neurotrophic factor (BDNF), and a Stroop color–word test evaluated attention capacity and processing speed.
Results: In the cross-sectional data, the serum vitamin C concentration was positively associated with the level of attention (r = 0.16, p = 0.02; standardized B = 0.21, p = 0.003), while no significant associations with the levels of fatigue and mood variables being found. In the RCT, compared to the placebo, the vitamin C supplementation significantly increased attention (p = 0.03) and work absorption (p = 0.03) with distinct tendency of improvement on fatigue (p = 0.06) and comprehensive work engagement (p = 0.07). The vitamin C supplementation did not affect mood and serum concentrations of BDNF. However, in the Stroop color–word test, the subjects supplemented with vitamin C showed better performance than those in the placebo group (p = 0.04).
Conclusions: Inadequate vitamin C status is related to a low level of mental vitality. Vitamin C supplementation effectively increased work motivation and attentional focus and contributed to better performance on cognitive tasks requiring sustained attention.
Source: https://doi.org/10.1007/s00394-021-02656-3
Extreme Fatigue
Extreme Fatigue refers to lack of energy or tiredness of whole body. There are many causes of Extreme fatigue such as alcohol and other drugs.
EXAMPLE CASE STUDY:
A 37-year-old female presented with digestive complaints, carb cravings, ‘overwhelming fatigue’, trouble concentrating at work, and unable to play with her daughter after work due to feeling tired all the time.
She couldn’t remember feeling ‘normal’ since before she had her daughter 6 years ago. She did not have difficulty falling asleep and often went to bed as early as 8pm. However she often woke during the night and could not fall back asleep due to ‘over-thinking’.
She had also been struggling to reduce her weight and had actually been gaining weight for the past 6 years. She complained of reflux, heaviness and discomfort after meals, especially those containing fat (which she has long tried to avoid in her diet), explaining that this may have something to do with her having her gall bladder removed a few years prior.
Treatment
She was prescribed a compounded mixture of 1,500 mg of Taurine (to assist with bile flow, metabolism of fats, support for detoxification & potentially weight management), and 200mg of 5-HTP (to support her sleep & appetite cravings).
The patient was also supported to cut out take-away/junk foods & sugary drinks, and advised not to consume caffeine after 12 pm.
She was also advised to quit her after-work wine habit and exercise every morning (yoga, walking).
Outcome
After just 2 weeks of treatment, the patient reported that although the first few days of changing her habits was hard, she had started feeling a lot better after just 1 week. After 2 weeks, not only did she have more energy, she reported getting a ‘rumbly tummy’ once again whenever she got hungry, and felt that she digested food more completely, feeling ‘lighter’ and more regular. She also reported better sleep.
As her digestive capacity had improved she was prescribed a daily teaspoon of Arctic Cod Liver Oil (divided into half at breakfast and dinner, to help supply natural Vitamin A and D as fat-soluble nutrients she was deficient in, from her long standing fat malabsorption) and continuation of another batch of the compounded Taurine/5-HTP formula mixture.
After 4 weeks, her improved fat-soluble detoxification may have assisted with the increased energy she felt, as well as her self-reported ‘hormonal balance’.
offered to ‘boost’ her next script of compounded formula with some added Acetyl-Carnitine, to provide even further support for fat metabolism on a cellular level (helping mitochondria break down fat for energy).
She is excited to continue making more changes in her life thanks to the great improvements in her wellbeing that she has experienced, and is starting to plan a holiday with her young family.
Mechanisms of Action
Taurine
Taurine is a substrate for Bile Synthesis, fat metabolism and Phase II conjugation directly.
(Key to those seeking to support liver health, as well as assisting those working on hormone and toxin excretion, as well as better assimilation of Omega 3 EFAs, Vitamin D and A from the diet and supplements.)
Taurine may also assist in body fat reduction by reducing central adiposity and increasing insulin sensitivity, providing key support in type 2 diabetes and metabolic syndrome.
Supplementing Taurine can have a calming effect on nervous system allowing better nervous system balance and rest (by increasing activity of the GAD enzyme responsible for decreasing Glutamates, and can directly stimulate GABA receptors). Taurine deficiency in neuronal cells will therefore make them more prone to over-excitation.
5-HTP
5-HTP is an intermediate precursor to Serotonin in the body. It is used clinically to support balanced neurotransmitters, mood, sleep (by increasing the length of REM sleep), & appetite (by managing carbohydrate cravings, satiety and digestive regularity).