Mon - Thursday: 9.30am - 5.30pm - Most Saturdays - 9am - 1pm
Hashimoto’s Healing
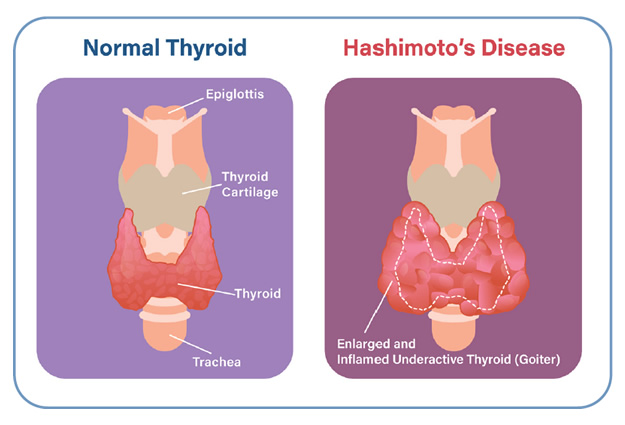
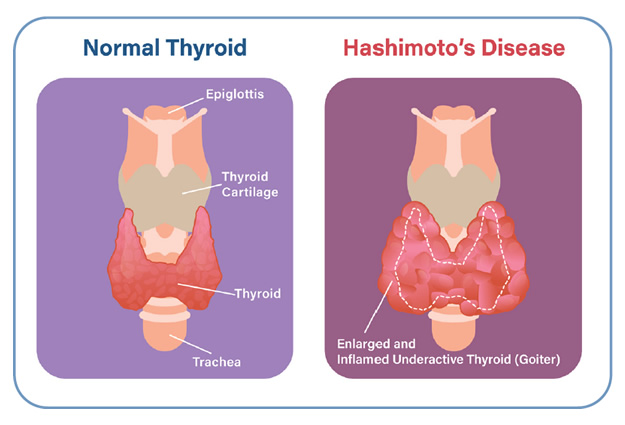
Hashimoto’s disease is an autoimmune condition where the immune system mistakenly attacks the thyroid gland. … Hypothyroidism is a condition in which the thyroid is not releasing enough of the two main hormones it produces, T3 (triiodothyronine) and T4 (thyroxine).
WELL-BEINGTOXINSIMMUNE SYSTEMSCIENCEHASHIMOTO'SFATIGUE STRESSSTRESS & ANXIETY
Benjamin McAvoy
11/11/20246 min read
Hashimoto’s Healing
Do you feel depressed?
Do you feel like you’ll never get better?
Is your weight creeping up, no matter what you do?
Is your energy at a zero, and it feels like it can’t get any worse?
Have your antibodies skyrocketed, and you don’t know what to do next?
Are you short-tempered with loved ones despite your best efforts?
Has brain fog stolen your ability to think?
Do family and friends misunderstand that you’re trying to get better?
Is your hair thinning all over and you’re worried you won’t have much left?
Has your anxiety taken over your life?
Have you been to numerous doctors, allergists, endocrinologists, even natural doctors, who don’t know what to do with you?
Can Hashimoto's be cured.?
There is no cure for Hashimoto’s thyroiditis. (so modern medicine thinks) The timeframe of the autoimmune process and inflammation will continue is not predictable. … Thyroid hormone medication can replace the hormones the thyroid made before the inflammation started. There are two major thyroid hormones made by a healthy gland (T3 and T4) It will also depend on if patients have no T3 + T4 issues. then we would have to work on TSH and Antibody reduction plan
What not to eat when you have Hashimoto's?
Myth 1: Goitrogens need to be avoided in Hashimoto’s, so I can’t eat broccoli. Those poor cruciferous vegetables! Delicious and healthy vegetables like cabbage, Brussels sprouts, broccoli, kale, and cauliflower have gotten a bad rap due to some old nomenclature and outdated patterns in thyroid disease. Myth 2: This will only depend on what diet you are currently eating, are you plant based, dairy free, sugar free, stress free.?
What's the difference between hashimoto's and hypothyroid ?
Hashimoto’s disease is an autoimmune condition where the immune system mistakenly attacks the thyroid gland. … Hypothyroidism is a condition in which the thyroid is not releasing enough of the two main hormones it produces, T3 (triiodothyronine) and T4 (thyroxine).
What does hashimoto's disease do to the body?
Hashimoto’s disease is an autoimmune condition where the immune system mistakenly attacks the thyroid gland. … Hypothyroidism is a condition in which the thyroid is not releasing enough of the two main hormones it produces, T3 (triiodothyronine) and T4 (thyroxine).
How does Hashimoto's effect the brain?
There are two ways Hashimoto’s can affect brain health. First, many people with Hashimoto’s also have an autoimmune attack against their nervous system. … second, Hashimoto’s can lead to low thyroid hormones, which are necessary to dampen the brain inflammation.
Does everyone have elevated Antibodies.?
In some people, the immune system makes antibodies that affect the thyroid gland. This causes health problems. These antibodies may target: … Almost everyone with Hashimoto’s thyroiditis has high levels of antibodies against TPO and Tg.
Can you have hashimoto's without a thyroid?
It’s possible to have Hashimoto’s thyroiditis for years without experiencing a single sign or symptom. But if you have symptoms, they will be associated with the disorder’s 2 primary complications—goiter and hypothyroidism. … With Hashimoto’s thyroiditis, hypothyroidism occurs much more often than a goiter
Hashimoto’s thyroiditis, or inflammation of the thyroid gland, is an autoimmune disorder. That means it is caused by a malfunction in your immune system. Instead of protecting your thyroid tissue, your immune cells attack it. These immune cells can cause hypothyroidism (underactive thyroid), a goiter (enlarged thyroid), or both. Eventually, the thyroiditis process can even destroy your entire thyroid, if left undetected or untreated. In Hashimoto’s thyroiditis, large amounts of damaged immune cells invade the thyroid. These immune cells are called lymphocytes; this is where Hashimoto’s other name—chronic lymphocytic thyroiditis—is derived from. When these lymphocytes enter the thyroid, they destroy the cells, tissue, and blood vessels within the gland. The process of destroying the thyroid gland is a slow one, which is why many people who have Hashimoto’s thyroiditis go many years without any noticeable symptoms. You can read more about this in our article about the symptoms of Hashimoto’s thyroiditis.
Because the thyroid is essentially coming under attack from invading cells, it isn’t able to produce as much thyroid hormone as it normally would. Eventually, this causes hypothyroidism. And in extreme cases, the immune cells can cause the thyroid to become enlarged and inflamed to the point that it produces a visible mass in the neck—a goiter.
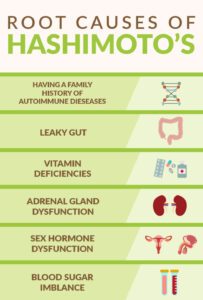
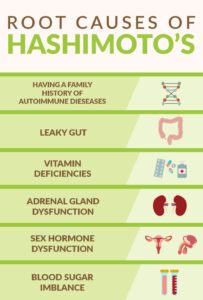
Doctors aren’t entirely sure why the immune system, which is supposed to defend the body from harmful viruses and bacteria, sometimes turns against the body’s healthy tissues. But what scientists do understand is that there are some factors that may make you more susceptible to this disease, and you can read about them in are article about risk factors for Hashimoto’s thyroiditis.
Hashimoto’s thyroiditis is an autoimmune disorder, so the main risk factor for developing this thyroid disorder is having a pre-existing autoimmune condition.
Autoimmune disorders occur when the body’s immune cells attack healthy tissue instead of protecting it. In the case of Hashimoto’s thyroiditis, immune cells attack the thyroid gland causing it to become inflamed and impairing its ability to produce enough thyroid hormone. You can read more about this in our article about what causes Hashimoto’s thyroiditis.
If you have an autoimmune disorder, your immune system is malfunctioning in some way. That’s why you are at a higher risk of developing Hashimoto’s thyroiditis than someone who does not have an autoimmune disorder.
Below are examples of common autoimmune disorders:
Addison’s disease
Rheumatoid arthritis
Type 1diabetes
If you have an autoimmune disorder, that is a risk factor for developing Hashimoto’s thyroiditis. That’s why you should get checked for Hashimoto’s thyroiditis every once in a while (your doctor will determine exactly how often you should get tested). That way, you will have the best chance of getting the disease detected early on
In addition to conducting a physical examination and taking your unique symptoms into account, your doctor / Benjamin will use one or more laboratory tests to diagnose Hashimoto’s thyroiditis. This article will cover the 3 most common diagnostic tests that detect this common thyroid disorder: the thyroid-stimulating hormone test, anti-thyroid antibodies tests, and the free T4 hormone test.
A thyroid-stimulating hormone (TSH) test is a blood test that is one of the go-to tests for diagnosing hypothyroidism. Remember, Hashimoto’s thyroiditis is the most common cause of hypothyroidism.
Thyroid-stimulating hormone is not produced by your thyroid—it’s produced by your pituitary gland in your brain. When the pituitary detects even the slightest decrease in thyroid hormone production, it releases a greater amount of TSH to encourage the thyroid gland to make more hormones.
The goal of the TSH test is to determine whether your TSH levels are within the normal range. If they are higher than they should be, this may indicate Hashimoto’s thyroiditis (and, in turn, hypothyroidism). Remember, higher TSH levels mean that your brain thinks the thyroid is not producing enough hormones and needs stimulation (the “S” in TSH) to make more. Thyroid-stimulating hormone ranges are unique to each patient, and your doctor will determine your healthy TSH range.
Anti-thyroid antibodies (ATA) tests, such as the microsomal antibody test (also known as thyroid peroxidase antibody test) and the anti-thyroglobulin antibody test, are commonly used to detect the presence of Hashimoto’s thyroiditis.
Hashimoto’s thyroiditis is an autoimmune disorder, and these types of disorders are caused by immune system malfunction. In other words, instead of protecting the body’s healthy tissues, malfunctioning immune cells actually attack them.
When immune cells attack your thyroid gland, which is the case with Hashimoto’s thyroiditis, antibodies are produced. Anti-thyroid antibodies tests detect the presence of these antibodies and measure their levels. This test is commonly used to confirm or exclude Hashimoto’s thyroiditis as the reason for hypothyroidism.
Autoimmune disorders are caused by a malfunction in your immune system. Hashimoto’s thyroiditis is an autoimmune disorder, which is why the primary complication associated with Hashimoto’s thyroiditis is that it increases your risk of developing other autoimmune disorders.
Hashimoto’s thyroiditis increases your risk of developing a number of autoimmune disorders.
Some examples include:
Addison’s disease
Graves’ disease
premature ovarian failure
type 1 diabetes
lupus erythematosus (a disorder that causes inflammation in a number of the body’s systems, including the lungs and heart)
pernicious anemia (a disorder that prevents the absorption of vitamin B12)
rheumatoid arthritis
thrombocytopenic purpura (a disorder that interferes with the blood’s ability to clot)
vitiligo (a disorder that produces white patches on the skin due to attacks on skin pigment cells)
It’s a very rare complication, but Hashimoto’s thyroiditis may increase your risk of developing a specific kind of thyroid cancer known as thyroid lymphoma. Thyroid lymphoma is highly treatable and curable when it’s detected early on. That’s why it’s so important to pay attention to any thyroid nodules (or thyroid lumps) and get them examined by your doctor as soon as possible.
Because Hashimoto’s thyroiditis can increase your risk for certain autoimmune disorders, you should talk to your doctor about what steps you should take to effectively manage these risks. Your doctor may recommend periodic tests to ensure that any associated complication is detected—and treated—as early as possible.
© 2004 - 2026. All rights reserved. Benjamin McAvoy Integrative Naturopath


Recent Posts by Benjamin
Top 8 Uses of Low Dose Naltrexone (LDN) + Side Effects
Measles Virus Wipes Out Golf-Ball-Sized Cancer Tumor In 36 Hours
Ginger Tea: Dissolves Kidneys Stones, Cleanses Liver And Reduce Joint Pain
Weedkiller 'raises risk of non-Hodgkin lymphoma by 41%'
Unvaccinated Children's pose zero risk to anyone-Harvard immunologist
Benjamin Mcavoy
Email : Message Here (Use contact form)
Phone : 0422225151
Address : Settlers Blvd - Chisholm NSW 2322 Australia
Hours: Mon – Fri : 9.30am – 4.30pm
Day: Sat : 9am – 12pm - Alternate Saturday's
